Table of Contents
Introduction
Did you know that up to 30% of people taking antibiotics experience gastrointestinal side effects such as diarrhea? This staggering statistic highlights the delicate balance of our gut microbiome, which can be thrown off course by antibiotic use. When we think of antibiotics, we often focus on their ability to combat harmful bacteria. However, these powerful medications don’t discriminate—they also affect the beneficial bacteria that play a crucial role in our overall health.
As we navigate the complexities of gut health, one question arises: When should we take probiotics in relation to antibiotics? This blog post aims to demystify the relationship between these two elements and provide you with clear guidelines to support your gut health during antibiotic treatment.
We’ll explore the mechanisms of probiotics, their potential benefits when paired with antibiotics, and the best practices for incorporating them into your routine. Here at Bala Health, we are committed to empowering our customers with science-backed information, so you can make informed decisions about your health. By the end of this post, you will understand how to effectively use probiotics to help maintain your gut health while undergoing antibiotic treatment.
Let’s dive into the fascinating world of probiotics and antibiotics, and uncover how we can support our gut health through informed choices.
Understanding Antibiotics and Their Impact on Gut Health
The Role of Antibiotics
Antibiotics are medications designed to destroy or inhibit the growth of bacteria. They are commonly prescribed for bacterial infections, helping to alleviate symptoms and prevent complications. While antibiotics can be lifesaving, they also have a downside: they disrupt the natural balance of microorganisms in our gut.
The Gut Microbiome
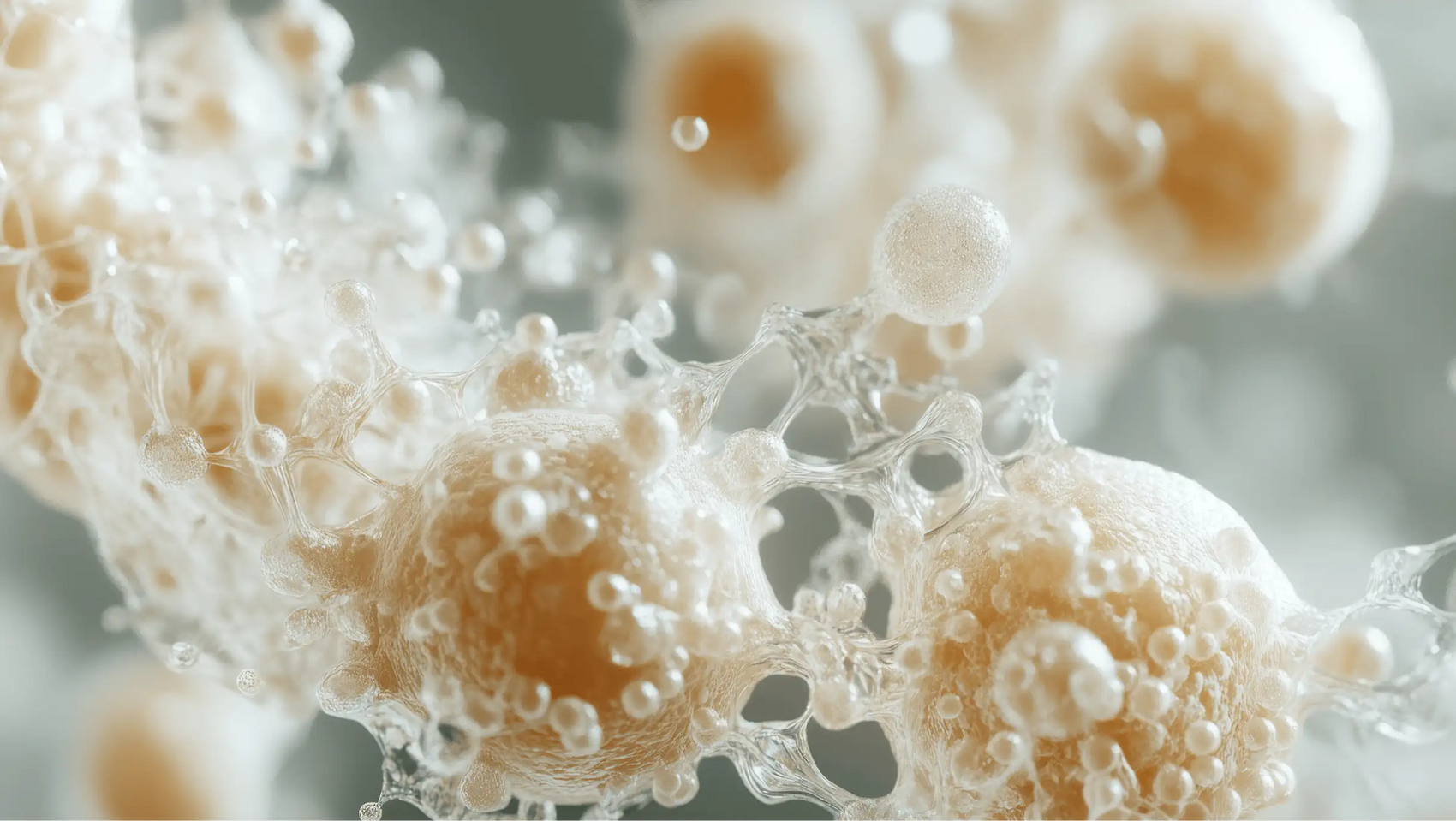
Our gut is home to trillions of microorganisms, collectively known as the gut microbiome. This diverse community of bacteria, fungi, and viruses plays a vital role in our overall health, influencing digestion, metabolism, and even immune function. A healthy gut microbiome is characterized by a diverse array of beneficial bacteria that work together to maintain balance and support our bodily functions.
The Disruption Caused by Antibiotics
When we take antibiotics, they indiscriminately kill both harmful and beneficial bacteria. This disruption can lead to a reduction in microbial diversity, making us more susceptible to gastrointestinal issues, infections, and other health complications. Research has shown that this imbalance can persist long after the antibiotic course has ended, affecting our gut health for months or even years.
Probiotics: The Gut's Friendly Allies
What Are Probiotics?
Probiotics are live microorganisms, often referred to as "good" or "friendly" bacteria, that confer health benefits when consumed in adequate amounts. They help restore the balance of the gut microbiome by replenishing beneficial bacteria that may have been lost during antibiotic treatment. Probiotics are available in various forms, including supplements and fermented foods such as yogurt, kefir, sauerkraut, and kimchi.
How Do Probiotics Work?
Probiotics exert their beneficial effects through several mechanisms:
- Restoring Microbial Balance: Probiotics can help replenish beneficial bacteria in the gut, restoring the balance disrupted by antibiotics.
- Competing with Pathogens: Probiotics can outcompete harmful bacteria for resources, reducing the risk of infections.
- Modulating Immune Response: Probiotics can help regulate the immune response, promoting a healthy inflammatory response in the gut.
- Producing Short-Chain Fatty Acids (SCFAs): Certain probiotic strains produce SCFAs, which provide energy for gut cells and have anti-inflammatory properties.
When to Take Probiotics with Antibiotics
Timing Matters
The timing of probiotic consumption in relation to antibiotics is crucial for maximizing their benefits. Here are our recommendations:
- Start Early: We suggest starting probiotics on the same day you begin your antibiotic treatment. This approach helps mitigate the initial disruption to your gut microbiome.
- Continue During Treatment: Continue taking probiotics throughout the entire course of antibiotics to support your gut health.
- Post-Antibiotic Phase: It’s beneficial to continue taking probiotics for at least two weeks after completing your antibiotic course. This helps ensure that your gut microbiome has the best chance of recovering and reestablishing a healthy balance.
Separation of Doses
To avoid potential interactions, we recommend separating the doses of your antibiotics and probiotics by at least two hours. This ensures that the probiotic bacteria have a better chance of surviving and colonizing your gut without being affected by the antibiotic.
Choosing the Right Probiotics
Not all probiotics are created equal, and it's essential to choose high-quality, science-backed strains. Look for probiotics that contain well-studied strains such as:
- Lactobacillus rhamnosus GG (LGG): Known for its effectiveness in restoring gut flora balance during and after antibiotic use.
- Bifidobacterium animalis subsp. lactis (BB-12): Shown to enhance the recovery of gut microbe populations after antibiotic use.
- Saccharomyces boulardii: A yeast probiotic that has been found effective in reducing the risk of antibiotic-associated diarrhea.
At Bala Health, our flagship probiotics are designed with these clinically validated strains to support gut health effectively. You can explore our offerings here.
The Science Behind Probiotics and Antibiotics
Clinical Evidence Supporting Probiotic Use
Numerous studies have demonstrated the benefits of taking probiotics during antibiotic treatment. A meta-analysis concluded that probiotics significantly reduce the risk of antibiotic-associated diarrhea (AAD). In fact, taking probiotics during antibiotic therapy can lower the incidence of AAD from 19% to about 8%.
Probiotics not only help mitigate gastrointestinal symptoms but also aid in preserving the diversity of gut flora that antibiotics may disrupt. This preservation is vital for overall gut health and can help prevent long-term complications associated with antibiotic use.
Exploring the Controversies
While many studies support the use of probiotics with antibiotics, some researchers argue that the evidence is not yet conclusive. They highlight the variability in probiotic strains and formulations, leading to inconsistent results. It’s essential to approach the topic with an open mind and rely on high-quality, evidence-based products like those from Bala Health.
Incorporating Probiotics into Your Routine
Tips for Optimal Use
To get the most out of your probiotics while on antibiotics, consider the following tips:
- Consistency is Key: Take your probiotics at the same time every day to establish a routine.
- Stay Hydrated: Adequate hydration supports the overall health of your gut microbiome.
- Pair with Prebiotics: Include prebiotic-rich foods in your diet, such as garlic, onions, and bananas. Prebiotics serve as food for probiotics, enhancing their effectiveness.
- Monitor Your Body's Response: Pay attention to how your body responds to probiotics, and consult a healthcare professional if you experience any adverse effects.
Conclusion
Navigating the world of antibiotics and probiotics doesn’t have to be complicated. By understanding when to take probiotics with antibiotics, we can better support our gut health and mitigate the side effects of antibiotic use. Starting probiotics on the same day you begin antibiotics, continuing throughout treatment, and for two weeks afterward will help restore balance to your gut microbiome.
At Bala Health, we are dedicated to providing clean, science-backed probiotics to help you feel better from the inside out. If you’re ready to take the next step in supporting your gut health, we invite you to take our 3-minute Weight-Loss Quiz to find your personalized gut-health roadmap. And don’t forget to check out our clinically-backed probiotics here to kick-start your journey to better gut health.
FAQ
1. Can I take probiotics with any antibiotic?
Yes, probiotics can be taken with most antibiotics, but it’s essential to separate the doses by at least two hours to ensure the probiotics have the best chance of survival.
2. How long should I take probiotics after finishing antibiotics?
It’s recommended to continue taking probiotics for at least two weeks after completing your antibiotic course to support gut recovery.
3. Are all probiotics effective?
Not all probiotics are created equal. Look for those with clinically validated strains, such as Lactobacillus rhamnosus GG or Bifidobacterium animalis lactis, for optimal results.
4. Can I get enough probiotics from food alone?
While fermented foods like yogurt and sauerkraut can provide beneficial bacteria, they may not deliver a therapeutic dose necessary to counteract the effects of antibiotics. High-quality probiotic supplements, like those from Bala Health, can provide more effective support.
5. What should I do if I experience gastrointestinal side effects while on antibiotics?
If you encounter side effects such as diarrhea or bloating while taking antibiotics, consider consulting a healthcare professional. They may advise you on the appropriate use of probiotics and how to best support your gut health.