Table of Contents
Introduction
Did you know that a significant percentage of people taking antibiotics experience gastrointestinal side effects? According to research, more than a third of individuals may suffer from issues like diarrhea or bloating during their antibiotic course. As we navigate our health journeys, understanding the connection between antibiotics and gut health becomes increasingly vital. The gut microbiome, a complex ecosystem of microorganisms residing in our intestines, plays a crucial role in our overall wellness, influencing everything from digestion to immune function.
In this blog post, we will explore the optimal timing for taking probiotics alongside antibiotics, the types of probiotic strains that are most beneficial, and how we can mitigate the side effects associated with antibiotic use. Our aim is to empower you with knowledge, helping you make informed decisions about your gut health, especially during times when you might need antibiotics. At Bala Health, we are committed to providing clean, science-backed probiotics that work effectively, supporting your journey towards better health from the inside out.
So, are you tired of the confusion surrounding probiotics and antibiotics? Perhaps you've wondered, "When should I take my probiotics?" or "Will they even help?" You’re not alone! Let’s delve into the science behind probiotics and antibiotics, unravel the best practices, and clarify any misconceptions.
Understanding Antibiotics and Their Impact on Gut Health
Antibiotics are powerful medications designed to combat bacterial infections. They work by targeting and killing harmful bacteria; however, they cannot distinguish between good and bad bacteria, leading to a significant disruption in our gut microbiome. This disruption, known as dysbiosis, can result in a decreased diversity of beneficial bacteria, which is essential for maintaining gut health.
The Role of Gut Microbiome
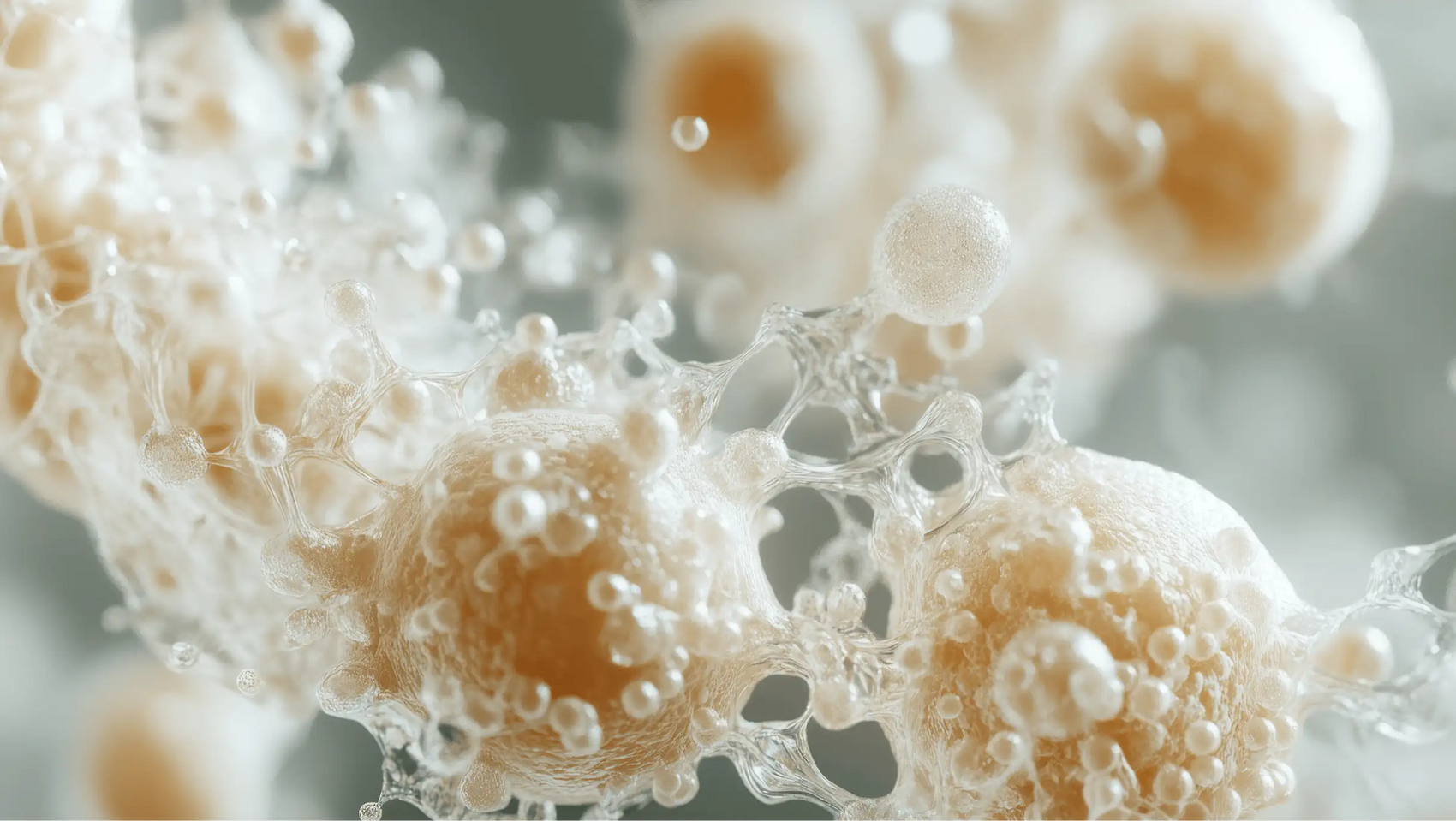
The gut microbiome consists of trillions of microorganisms, including bacteria, fungi, and viruses, that work in harmony to keep our digestive system functioning optimally. When antibiotics are administered, they can severely deplete the population of these beneficial bacteria, leading not only to digestive issues but also to long-term health consequences such as increased risk of infections, allergies, and even mental health issues.
Common Side Effects of Antibiotics
When taking antibiotics, many individuals experience:
- Diarrhea: This is one of the most common side effects, occurring due to the imbalance created in the gut.
- Bloating: An uncomfortable feeling of fullness that can accompany dietary changes or medication.
- Nausea: This can also disrupt your routine and lead to a loss of appetite.
- Vaginal Thrush: Antibiotics can disturb the natural balance of bacteria, leading to yeast overgrowth.
Understanding these potential side effects emphasizes the importance of taking probiotics during antibiotic treatment.
Probiotics: The Gut’s Best Friend
Probiotics are live microorganisms that provide health benefits when consumed in adequate amounts. They help restore balance to the gut microbiome, support digestive health, and may even enhance immune function. Taking probiotics during and after antibiotic treatment can mitigate some of the adverse effects and support gut restoration.
What Are the Best Probiotic Strains to Take with Antibiotics?
When looking for a probiotic to take alongside antibiotics, it is crucial to select strains that have been clinically proven to survive the harsh environment of the gut and exert beneficial effects. Some of the most researched probiotic strains include:
- Lactobacillus rhamnosus GG (LGG®): Well-studied for its ability to survive antibiotics and help reduce the risk of antibiotic-associated diarrhea.
- Bifidobacterium animalis subsp. lactis (BB12®): Known to enhance the recovery of gut bacteria following antibiotic use.
- Saccharomyces boulardii: A yeast probiotic that has shown efficacy in preventing diarrhea in individuals taking antibiotics.
These strains have demonstrated their ability to support gut health effectively, even during antibiotic treatment.
When is the Best Time to Take Probiotics with Antibiotics?
The timing of probiotic intake in relation to antibiotic dosing is essential for maximizing their benefits. Research suggests that the best practice is to take probiotics both during the course of antibiotics and for at least two weeks after completing the antibiotic course. But what specific timing should we consider?
Starting with Probiotics
For optimal results, we should start taking probiotics as soon as we begin our antibiotic treatment. This proactive approach allows beneficial bacteria to begin populating the gut while antibiotics are still active, helping to mitigate potential disruptions.
Timing Between Doses
To maximize the effectiveness of both antibiotics and probiotics, it is generally recommended to separate the doses by at least two hours. This timing helps ensure that the probiotics can function effectively within the gut without being compromised by the antibiotics.
- Example Schedule: If you take your antibiotic at 8 AM, consider taking your probiotic at 10 AM or later.
- Consistency is Key: Aim to take your probiotics at the same time every day to establish a routine and enhance adherence.
Probiotic Foods vs. Supplements
While incorporating probiotic-rich foods into our diets can be beneficial for gut health, they may not always provide the therapeutic doses needed to counteract antibiotic side effects effectively. Foods such as yogurt, kefir, sauerkraut, and kimchi contain beneficial bacteria, but the amounts may vary significantly, and they often do not meet the potency required during antibiotic treatment.
Why Choose Probiotic Supplements?
- Targeted Strains: Probiotic supplements can offer specific strains that have been clinically tested for effectiveness.
- Higher Potency: Supplements typically contain higher concentrations of probiotics compared to food sources, ensuring that you receive an adequate dose.
- Ease of Use: Supplements can be taken conveniently as part of your daily routine.
At Bala Health, we offer a clinically-backed probiotic that is designed for optimal gut health support, making it an excellent choice for those undergoing antibiotic treatment. Shop our clinically-backed probiotic now.
Post-Antibiotic Care: Continuing Probiotics
Once you finish your antibiotic course, continuing to take probiotics for at least two weeks can help restore the gut microbiome balance. This period is crucial for allowing beneficial bacteria to repopulate the gut and outcompete any potential harmful microbes that may have taken advantage of the disruption.
Long-Term Gut Health
After the initial recovery period, you can transition to a daily probiotic designed for maintenance of gut health. This proactive approach supports ongoing digestive health and immune function, helping you feel your best from the inside out.
Conclusion
Taking probiotics during and after a course of antibiotics is a scientifically supported strategy for maintaining gut health and minimizing the side effects associated with antibiotic use. By understanding when and how to take probiotics effectively, we can better support our gut microbiome and overall well-being.
At Bala Health, our mission is to simplify gut health with clean, effective probiotics that empower you on your wellness journey. Whether you're facing antibiotic treatment or simply looking for a daily boost for your gut health, we’ve got you covered.
Ready to take the next step in your gut health journey? Take our 3-minute Weight-Loss Quiz to find your personalized roadmap and start your journey to better gut health with our clinically backed probiotics today!
FAQ
Can I take probiotics at the same time as antibiotics?
Yes, certain strains of probiotics, like Lactobacillus rhamnosus GG, are effective when taken alongside antibiotics. However, it’s best to separate their doses by at least two hours for optimal efficacy.
What are the benefits of taking probiotics with antibiotics?
Taking probiotics during antibiotic treatment can help reduce the risk of digestive side effects, restore gut microbiome balance, and support overall gut health.
How long should I continue taking probiotics after antibiotics?
It’s generally recommended to continue taking probiotics for at least two weeks after finishing your antibiotic course to aid in restoring gut health.
Are probiotic foods as effective as supplements?
While probiotic-rich foods can benefit gut health, supplements typically contain higher concentrations of specific strains that have been studied and proven effective, making them a better option during antibiotic treatment.
What should I look for in a probiotic supplement?
Choose a probiotic that contains clinically validated strains, has a high CFU (colony-forming units) count, and is backed by research to ensure effectiveness. At Bala Health, we prioritize science-backed formulations to support your gut health.
By understanding the intricacies of probiotics and antibiotics, we empower ourselves to make informed health choices that support our overall well-being. Let’s take charge of our gut health together!