Table of Contents
Introduction
Did you know that antibiotics, while lifesaving, can significantly disrupt the delicate ecosystem of our gut? Recent studies show that antibiotics can wipe out beneficial bacteria alongside the harmful ones they target. This disruption has led many of us to ask: Do antibiotics ruin your gut health? As we navigate through a world increasingly reliant on these powerful medications, understanding their effects on our gut microbiome is more important than ever.
In recent years, awareness has surged regarding the gut-brain connection, gut health's influence on our immune system, and the role that microbiome diversity plays in overall well-being. We at Bala Health believe that knowledge empowers our customers to make informed decisions about their health. Our mission is to help individuals feel better from the inside out with clean, science-backed probiotics that support gut health.
In this blog post, we will explore the impact of antibiotics on gut health, examine the science behind this relationship, and discuss actionable steps you can take to support your microbiome before, during, and after antibiotic treatment. We will also highlight how our flagship probiotic can be a game-changer in restoring balance to your gut.
So, if you're struggling with gut health or simply want to understand the implications of antibiotic use better, you're in the right place. Let’s dive into the details of how antibiotics affect our gut microbiome and what we can do to mitigate these effects.
Understanding the Gut Microbiome
What is the Gut Microbiome?
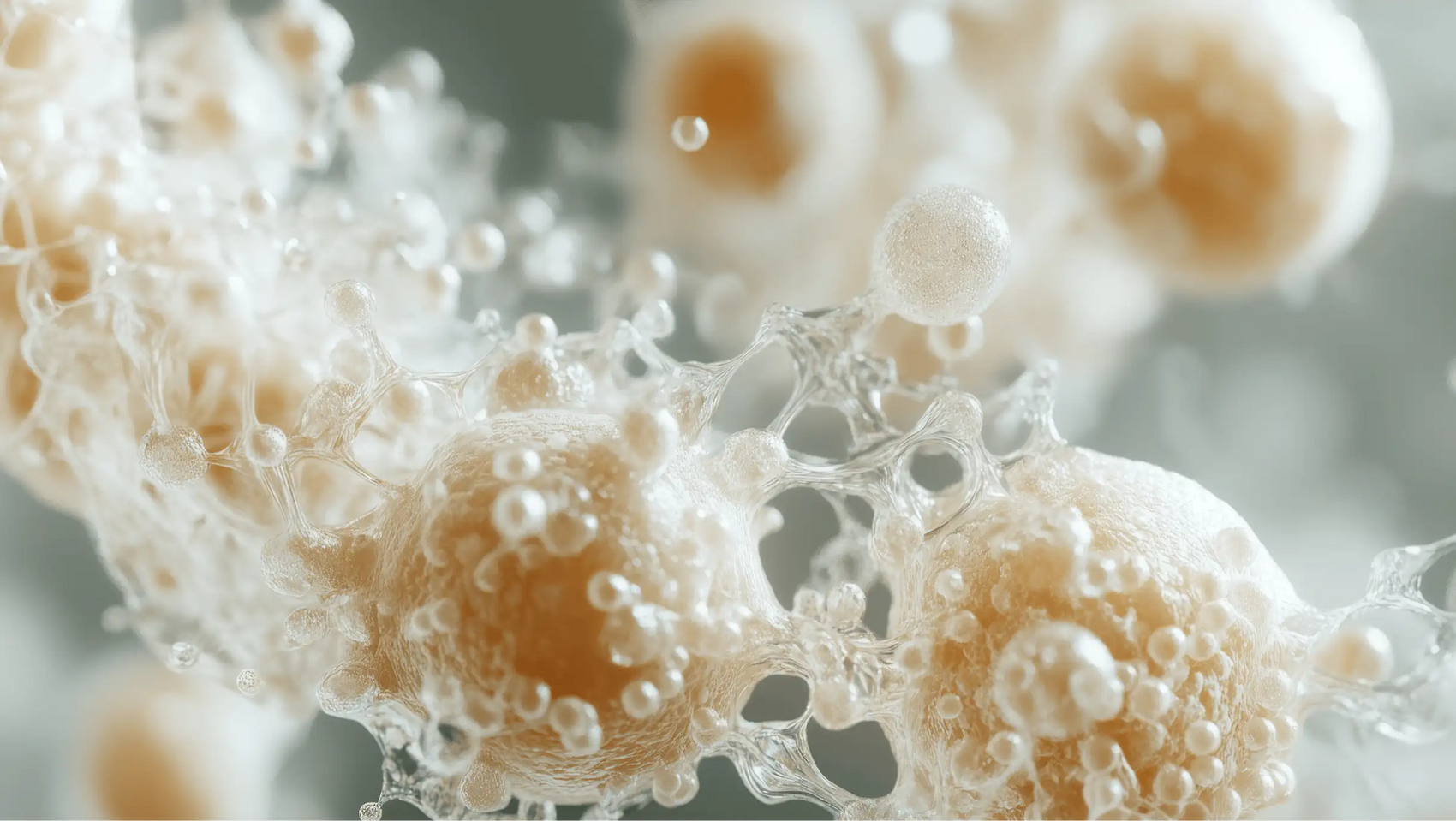
The gut microbiome comprises trillions of microorganisms, including bacteria, viruses, fungi, and other microbes, residing in our digestive tract. These microorganisms play essential roles in digestion, immune function, and even mental health. A diverse microbiome is crucial for overall health, as it helps:
- Digest food: Microbes break down complex carbohydrates and synthesize essential vitamins.
- Regulate the immune system: A balanced microbiome can prevent infections and inflammation.
- Support mental health: The gut-brain axis connects our digestive system with our brain, influencing mood and cognitive function.
The Importance of Microbiome Diversity
Diversity in the gut microbiome is vital for maintaining health. A rich variety of gut bacteria can enhance metabolic processes, support immune responses, and protect against pathogens. Studies have shown that individuals with a lower diversity of gut bacteria are at higher risk for conditions like obesity, diabetes, and gastrointestinal disorders.
Now, let’s turn our attention to antibiotics and their role in affecting this delicate balance.
The Role of Antibiotics in Gut Health
How Do Antibiotics Work?
Antibiotics function by targeting and killing bacteria that cause infections. However, they are not selective, meaning they can also affect beneficial bacteria in the gut. There are two primary types of antibiotics:
- Broad-spectrum antibiotics: These target a wide range of bacteria, both harmful and beneficial. Examples include amoxicillin and ciprofloxacin.
- Narrow-spectrum antibiotics: These are designed to target specific types of bacteria, causing less collateral damage to beneficial gut flora.
The Impact of Antibiotics on Gut Microbiome
Research indicates that antibiotics can lead to significant changes in gut microbiome composition, including:
- Reduction in microbial diversity: Antibiotics can drastically reduce the number of different bacteria species in the gut, leading to an imbalance known as dysbiosis.
- Increased risk of pathogenic overgrowth: With beneficial bacteria diminished, harmful bacteria like Clostridioides difficile can proliferate, potentially leading to severe gastrointestinal issues.
- Long-term effects: Some studies suggest that the changes in gut microbiome composition can persist for months or even years after antibiotic treatment.
Evidence from Research Studies
Recent studies found that after a course of antibiotics, the gut microbiome's diversity was affected as early as one day post-treatment and remained altered for up to six months. In some cases, certain beneficial bacteria never returned, leading to a long-term impact on gut health.
Recovery Strategies for Gut Health Post-Antibiotics
The Role of Probiotics
Probiotics are live microorganisms that can provide health benefits when consumed. They can help restore the balance of beneficial bacteria in the gut following antibiotic treatment. At Bala Health, we focus on clean, science-backed probiotics that adhere to our mission of transparency and integrity.
Our Probiotic Solution
Our flagship probiotic contains clinically validated strains designed to support gut health effectively. Incorporating our probiotics after antibiotic treatment may help ease occasional bloating and restore balance to your gut microbiome. Start your journey to better gut health—Shop our clinically-backed probiotic now.
The Importance of Prebiotics
Prebiotics are non-digestible food components that promote the growth of beneficial bacteria in the gut. Foods rich in fiber, such as fruits, vegetables, and whole grains, can serve as prebiotics. Including these in your diet can help nurture your gut microbiome and support recovery after antibiotic use.
Dietary Considerations
- Focus on a varied diet: Consuming a wide range of fruits, vegetables, and whole grains can enhance gut diversity.
- Include fermented foods: Foods like yogurt, kefir, and sauerkraut contain live cultures that can introduce beneficial bacteria to your gut.
- Avoid high-sugar and high-fat diets: These can promote the growth of harmful bacteria and negatively impact gut health.
Lifestyle Changes
- Stay hydrated: Adequate water intake supports digestion and overall gut health.
- Exercise regularly: Physical activity has been shown to enhance gut microbiome diversity.
- Manage stress: Stress management techniques, such as mindfulness and yoga, can positively affect gut health.
When Are Antibiotics Necessary?
While we recognize the potential risks of antibiotics, there are instances when they are essential for treating bacterial infections. It’s crucial to consult with a healthcare provider to determine the necessity of antibiotics and to explore alternatives when possible.
Additionally, we can take proactive measures to minimize the need for antibiotics in the first place. This includes:
- Practicing good hygiene: Washing hands frequently can help prevent infections.
- Staying up-to-date on vaccinations: Vaccines can protect against infections that may otherwise require antibiotics.
- Using antibiotics judiciously: Only take antibiotics when prescribed by a healthcare professional and complete the full course as directed.
Conclusion
In conclusion, while antibiotics play a crucial role in treating bacterial infections, their impact on gut health cannot be overlooked. They can disrupt the delicate balance of our gut microbiome, leading to long-lasting effects on our health. However, with the right strategies—such as incorporating probiotics, prebiotics, and maintaining a balanced diet—we can support and restore our gut health after antibiotic use.
At Bala Health, we are committed to empowering you with the knowledge and tools you need to take charge of your gut health. Kick-start your transformation—Take our 3-minute Weight-Loss Quiz to find your personalized gut-health roadmap, and feel better from the inside out—Subscribe & Save on our probiotics.
FAQ
1. Can antibiotics completely destroy my gut microbiome?
Antibiotics can significantly reduce the diversity of beneficial bacteria in your gut, but the extent of the damage varies depending on several factors, including the type of antibiotic used and the duration of treatment.
2. How long does it take for gut health to recover after antibiotics?
Gut microbiome recovery can vary; some studies indicate that diversity may take several months to return to baseline levels after antibiotic treatment.
3. Are all probiotics effective for restoring gut health after antibiotics?
Not all probiotics are created equal. Some strains have been shown to be more effective in restoring gut health post-antibiotic treatment, such as Saccharomyces boulardii and Lactobacillus rhamnosus GG.
4. Should I take probiotics during antibiotic treatment?
Consult with your healthcare provider. Some studies suggest that taking probiotics during antibiotic treatment may help mitigate some adverse effects.
5. How can I maintain gut health without antibiotics?
Maintaining good hygiene, eating a balanced diet rich in fiber and fermented foods, and staying active can help support a healthy gut microbiome.
We hope this comprehensive guide has helped illuminate the complexities of antibiotics and gut health. Remember, your gut health is a journey, and we’re here to support you every step of the way!