Table of Contents
Introduction
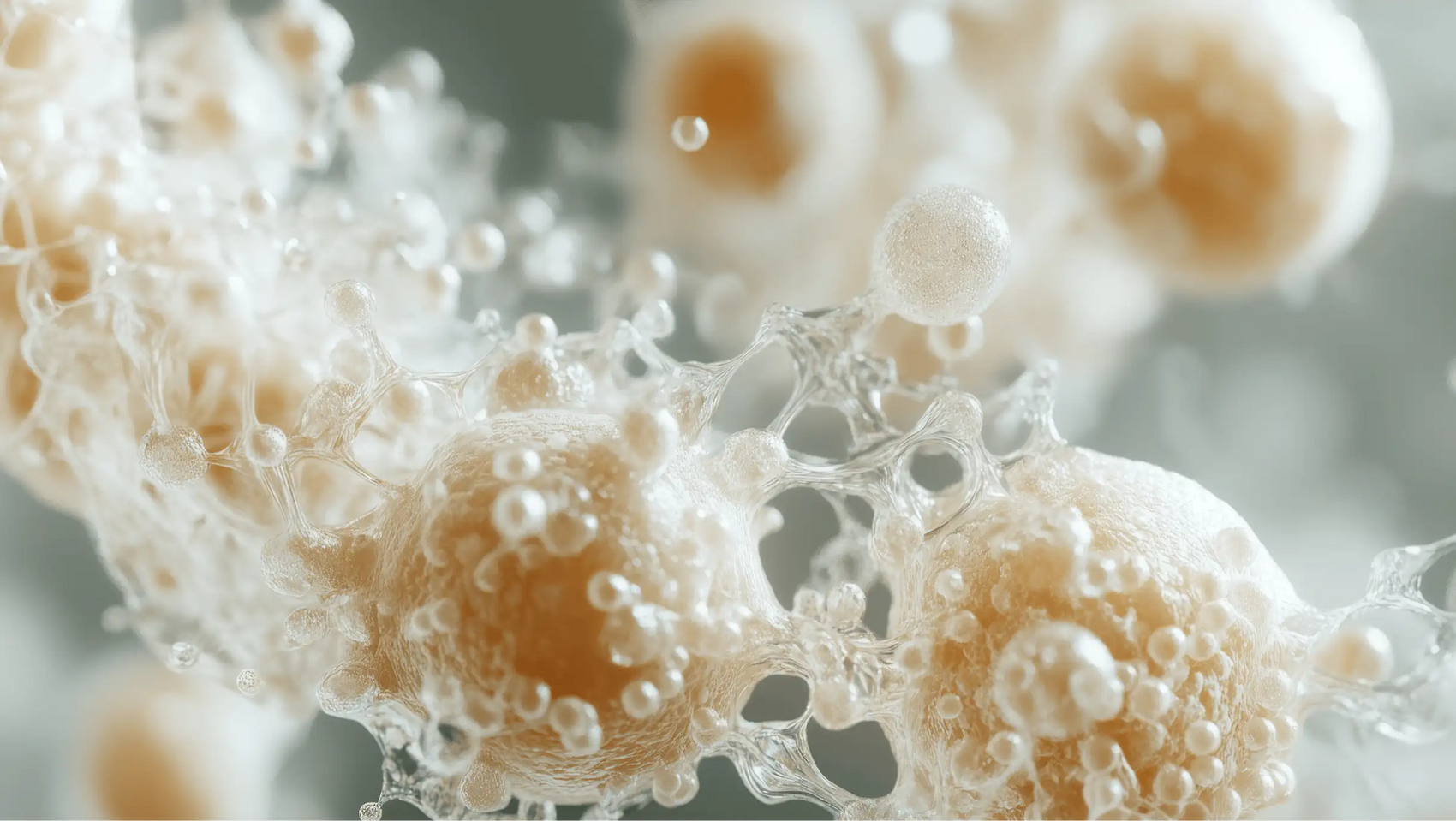
Did you know that your gut is home to trillions of bacteria, many of which play a crucial role in maintaining your overall health? Recent studies have shown that the gut microbiome is not just a collection of microbes; it’s a dynamic ecosystem that influences everything from digestion to immune function. However, when we turn to antibiotics to fight infections, we may inadvertently disrupt this delicate balance.
Antibiotics, while lifesaving, can have significant repercussions on our gut health. They are designed to eliminate harmful bacteria, but they often indiscriminately affect beneficial microbes as well. As a wellness brand committed to simplifying gut health, we at Bala Health recognize the importance of understanding how antibiotics interact with our microbiome and what we can do to mitigate their impact.
In this blog post, we will explore the intricate relationship between antibiotics and gut health. We will delve into the science behind how antibiotics affect our microbiome, the potential long-term consequences of these changes, and effective strategies for recovery after antibiotic use. By the end, you will have a comprehensive understanding of why maintaining gut health is essential and how our clean, science-backed probiotics can support your journey.
The Role of Antibiotics in Modern Medicine
Antibiotics have been a cornerstone of modern medicine for decades, revolutionizing the way we treat bacterial infections. They have saved countless lives by effectively combating diseases that were once fatal. However, the rise in antibiotic usage—an increase of 66% since 2000—has raised concerns among health professionals about their impact on our microbiomes.
How Antibiotics Work
Antibiotics target specific bacterial pathways to inhibit growth or kill bacteria. While this is effective for treating infections, it does not discriminate between harmful and beneficial bacteria. This collateral damage can lead to a phenomenon known as dysbiosis, where the balance of gut bacteria is disrupted.
Types of Antibiotics and Their Specifics
Different classes of antibiotics can have varying impacts on the gut microbiome:
- Broad-spectrum antibiotics such as amoxicillin and ciprofloxacin are particularly disruptive, as they target a wide range of bacteria, including beneficial strains.
- Narrow-spectrum antibiotics, on the other hand, are designed to target specific pathogens, potentially causing less disruption to the gut flora.
The choice of antibiotic, along with the duration of treatment, plays a significant role in determining the extent of microbial disruption.
The Impact of Antibiotics on Gut Microbiota
When we take antibiotics, the immediate effect is often a reduction in the diversity of our gut microbiota. This is concerning because a diverse microbiome is associated with better health outcomes and resilience against diseases.
Short-Term Effects
Research indicates that even a short course of antibiotics can lead to noticeable changes in the gut microbiome within days. For instance, studies have shown that antibiotic treatment can reduce the population of beneficial bacteria, leading to symptoms such as diarrhea, bloating, and gas—often referred to as antibiotic-associated diarrhea (AAD).
Long-Term Consequences
The long-term effects of antibiotic use can be more profound. Some studies suggest that alterations in the gut microbiome can persist for months, or even years, after completing a course of antibiotics. For instance:
- Decreased Microbial Diversity: A lack of diversity in gut bacteria has been linked to various health issues, including obesity, inflammatory bowel disease, and metabolic disorders.
- Increased Resistance Genes: The selective pressure from antibiotics can lead to an increase in antibiotic-resistant bacteria within the gut, posing a significant public health risk.
The implications of these changes extend beyond the gut itself; they can affect overall health, immune responses, and even mental well-being due to the gut-brain axis.
Strategies for Mitigating Antibiotic Impact
While it’s clear that antibiotics can disrupt gut health, there are proactive steps we can take to mitigate their effects. Here are some strategies we recommend:
1. Probiotics: A Promising Ally
Probiotics can play a vital role in restoring gut health after antibiotic use. These live microorganisms can help replenish beneficial bacteria and promote a balanced microbiome. However, not all probiotics are created equal. At Bala Health, we prioritize clinically validated strains that have been shown to support gut health effectively.
Our flagship probiotic can help ease occasional bloating and support a healthy immune system. Start your journey to better gut health – Subscribe & Save.
2. Prebiotics: The Food for Good Bacteria
In addition to probiotics, incorporating prebiotic-rich foods into your diet can aid in the recovery of your gut microbiome. Prebiotics are non-digestible food components that promote the growth of beneficial bacteria. Foods high in prebiotics include:
- Bananas
- Onions
- Garlic
- Asparagus
- Whole grains
A diet rich in fiber not only supports gut bacteria but also enhances overall digestive health.
3. Diverse and Balanced Diet
Eating a varied diet rich in fruits, vegetables, whole grains, and fermented foods can enhance gut microbiota diversity. Foods like yogurt, kefir, sauerkraut, and kimchi are excellent sources of beneficial bacteria that can help restore balance.
4. Limit Unnecessary Antibiotic Use
One of the most effective ways to protect gut health is to avoid unnecessary antibiotics. Antibiotics should only be prescribed when absolutely necessary and for bacterial infections. This approach can help preserve the delicate balance of your gut microbiome.
5. Hydration and Lifestyle Factors
Staying hydrated and engaging in regular physical activity can also contribute to a healthy gut. Physical activity has been shown to enhance gut microbial diversity, while proper hydration supports digestive processes.
6. Consider Timing of Probiotic Use
Research suggests that probiotics should ideally be taken during and after a course of antibiotics to maximize their effectiveness in restoring gut health. Incorporating our probiotic into your routine can help support your microbiome during this critical time.
Feel better from the inside out – Subscribe & Save.
The Science Behind Probiotics and Gut Recovery
The efficacy of probiotics in aiding gut recovery post-antibiotics is backed by science. Certain strains have demonstrated the ability to:
- Stimulate Short-Chain Fatty Acid Production: This is crucial for maintaining gut barrier integrity and reducing inflammation.
- Protect Resident Gut Microbiome: Probiotics can shield beneficial bacteria from being outcompeted by pathogens that may proliferate after antibiotic use.
- Support Immune Function: A balanced gut microbiome is essential for a healthy immune response.
Key Probiotic Strains to Consider
While many probiotics exist, the following strains have shown promising results in research:
- Lacticaseibacillus rhamnosus GG: Known for its ability to help prevent antibiotic-associated diarrhea.
- Saccharomyces boulardii: A yeast probiotic that has been effective in managing gastrointestinal health, especially during antibiotic treatment.
To make the most of these benefits, we recommend starting probiotics as soon as you begin antibiotic treatment and continuing for at least one week after completing the course.
Conclusion
The relationship between antibiotics and gut health is complex and multifaceted. While antibiotics are essential for treating bacterial infections, their impact on our gut microbiome cannot be overlooked. We must recognize the potential for long-term consequences, including decreased microbial diversity and increased antibiotic resistance.
However, by taking proactive steps—such as incorporating probiotics, prebiotics, and a balanced diet—we can support our gut health and mitigate the effects of antibiotic use. At Bala Health, we are dedicated to providing clean, science-backed probiotics that empower you on your wellness journey.
As you reflect on your health, consider taking the next step toward better gut health. Take our 3-minute Weight-Loss Quiz to find your personalized gut-health roadmap. Together, let’s work towards feeling better from the inside out.
FAQ
What are probiotics, and how do they help gut health?
Probiotics are live microorganisms that, when consumed in adequate amounts, can confer health benefits, particularly for gut health. They help restore balance to the gut microbiome, potentially easing digestive issues and supporting immune function.
Can I take probiotics while on antibiotics?
Yes, taking probiotics during and after a course of antibiotics can help mitigate the negative effects on your gut microbiome. It’s best to consult with a healthcare professional to determine the most suitable strains and timing for your needs.
How long does it take for gut health to recover after antibiotics?
Recovery time can vary depending on the individual and the antibiotic used. Some studies suggest that gut microbiome diversity can begin to recover within weeks, but full restoration may take several months.
Are there specific foods that can help restore gut health?
Yes! Foods high in prebiotics, such as bananas, onions, and garlic, as well as fermented foods like yogurt and sauerkraut, can help nourish beneficial gut bacteria and support recovery.
What steps can I take to maintain gut health during antibiotic use?
To maintain gut health, consider taking probiotics, eating a varied and balanced diet rich in fiber and prebiotics, staying hydrated, and engaging in regular physical activity. Avoid unnecessary antibiotics whenever possible.
By understanding the impact of antibiotics on gut health and incorporating effective strategies for recovery, we can take charge of our wellness journey and promote a thriving microbiome.