Table of Contents
- Introduction
- The Gut Microbiome: A Complex Ecosystem
- How Antibiotics Affect the Gut Microbiome
- The Role of Probiotics During Antibiotic Treatment
- Best Practices for Taking Probiotics with Antibiotics
- The Science Behind Probiotics and Antibiotics: What the Research Says
- Common Side Effects of Probiotics
- Empowering Your Gut Health Journey
- Conclusion
- FAQ
Introduction
Did you know that the human gut contains approximately 100 trillion microorganisms, comprising a complex ecosystem known as the gut microbiome? This intricate balance of bacteria is crucial for our overall health, influencing everything from digestion to immune function. However, when we take antibiotics to fight bacterial infections, the good bacteria in our gut can be significantly affected, leading to unwanted side effects like diarrhea and bloating.
Are you tired of the confusion surrounding gut health and the use of probiotics? You’re not alone. Many of us struggle with questions about how to maintain a healthy gut, particularly when antibiotics come into play. This blog post aims to clarify whether we can safely take probiotics alongside antibiotics and the best practices for doing so.
Throughout this post, we will delve into the science behind how antibiotics impact our gut microbiome, the role probiotics can play during and after antibiotic treatment, and which specific strains offer the most benefit. We are committed to providing clear, evidence-based information that empowers you to make informed decisions about your health—just as we do with our clean, science-backed probiotics at Bala Health.
We invite you to join us on this journey to better understand the relationship between antibiotics and probiotics, and explore how we can support our gut health in the process.
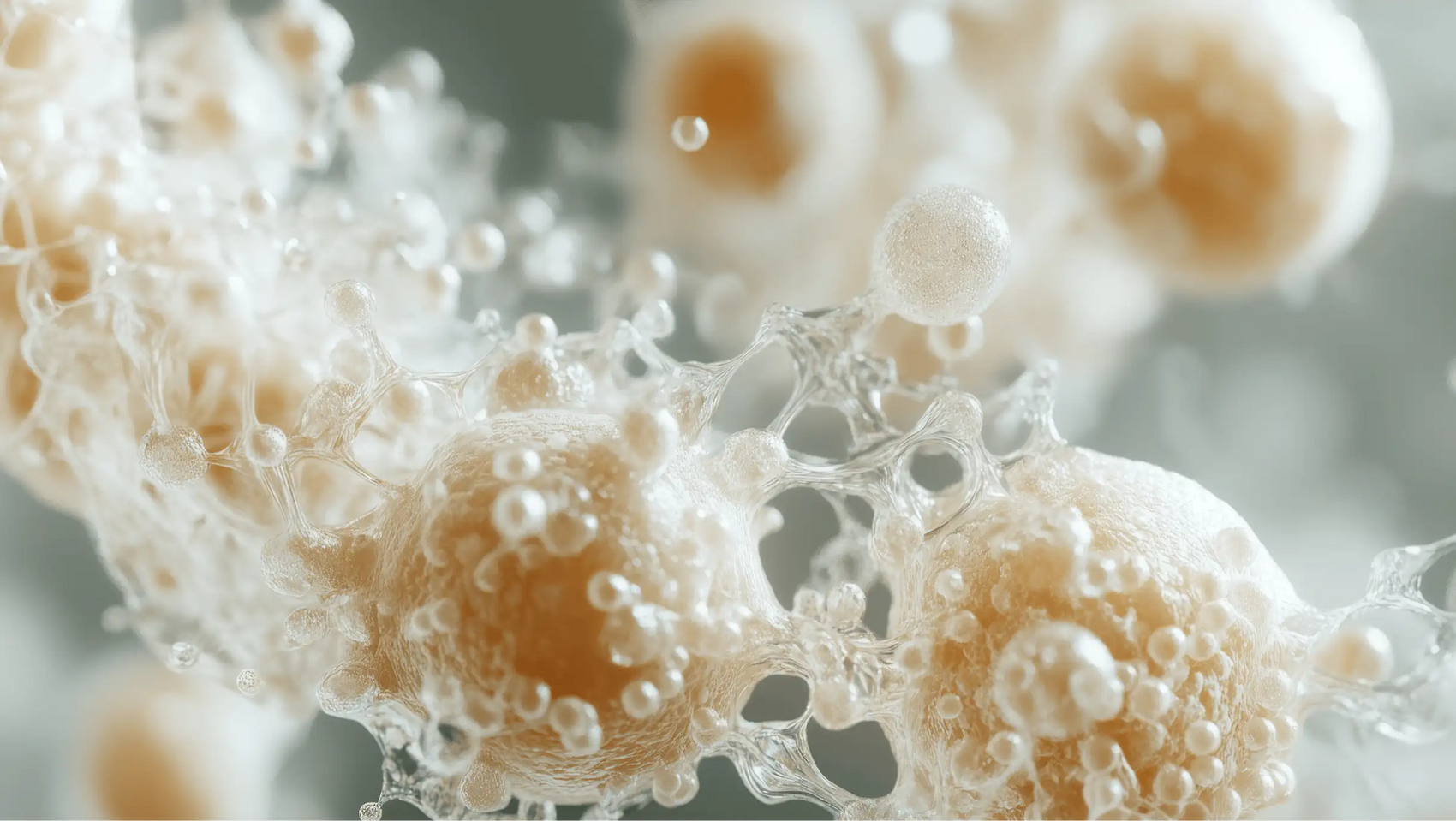
The Gut Microbiome: A Complex Ecosystem
The gut microbiome is a dynamic community of trillions of microorganisms, including bacteria, fungi, viruses, and protozoa, that inhabit our gastrointestinal tract. This diverse community plays numerous essential roles in our health, such as:
- Digesting food: Helping break down complex carbohydrates and fibers.
- Synthesizing vitamins: Producing vital nutrients like vitamin K and some B vitamins.
- Regulating the immune system: Contributing to our body's immune response and preventing infections.
- Affecting mood and mental health: The gut-brain axis connects our gut health to our mental well-being.
However, this delicate ecosystem can be disrupted by various factors, with antibiotic use being one of the most significant.
How Antibiotics Affect the Gut Microbiome
Antibiotics are designed to target and kill harmful bacteria that cause infections. However, they are not selective and often kill beneficial bacteria in the process. This indiscriminate action can lead to:
- Reduced microbial diversity: A healthy microbiome consists of a wide variety of bacteria. Antibiotics can significantly diminish this diversity, leading to an imbalance in gut flora.
- Antibiotic-associated diarrhea (AAD): This is a common side effect that can occur in 5% to 39% of antibiotic users, depending on the specific antibiotic prescribed. It is often caused by the overgrowth of harmful bacteria, such as Clostridium difficile, which can thrive when beneficial bacteria are depleted.
Research has shown that the gut microbiome can take several weeks to return to its original state after antibiotic treatment. This prolonged disruption can lead to ongoing digestive issues, making it crucial to find ways to support gut health during and after antibiotic use.
The Role of Probiotics During Antibiotic Treatment
Probiotics are live microorganisms that can confer health benefits when consumed in adequate amounts. They are often referred to as "good" or "helpful" bacteria. One of the primary reasons for taking probiotics during antibiotic treatment is to counteract the negative effects of antibiotics on the gut microbiome.
Benefits of Taking Probiotics with Antibiotics
- Preventing Antibiotic-Associated Diarrhea (AAD): Studies have shown that probiotics can significantly reduce the incidence of AAD. A meta-analysis of multiple studies indicated that probiotics reduced the risk of AAD by about 64%.
- Restoring Gut Balance: Probiotics can help replenish the beneficial bacteria that antibiotics may have killed, aiding in the restoration of a healthy gut microbiome.
- Improving Antibiotic Efficacy: Some research suggests that probiotics may enhance the effectiveness of certain antibiotics, particularly in the treatment of specific infections like Helicobacter pylori.
Best Practices for Taking Probiotics with Antibiotics
If you decide to take probiotics while on antibiotics, it's essential to do so correctly to maximize their benefits. Here are some best practices:
Timing Matters
To avoid potential interactions, it’s advisable to space out the timing of your antibiotic and probiotic doses:
- Take probiotics at least two hours apart from antibiotics: This allows the probiotic to reach the gut without interference from the antibiotic’s action.
Choosing the Right Probiotic Strains
Not all probiotics are created equal. Certain strains have been shown to be effective during antibiotic treatment. Look for probiotics that contain:
- Lactobacillus rhamnosus: This strain has been extensively studied and is known for its ability to survive antibiotic treatment and help maintain gut health.
- Saccharomyces boulardii: A beneficial yeast that is particularly effective in preventing AAD.
- Bifidobacterium species: Various strains of Bifidobacterium are also beneficial for gut health.
When selecting a probiotic, consider one that provides at least 5 to 40 billion colony-forming units (CFUs) per serving, depending on the specific strain and your individual health needs.
Continuing After Antibiotic Treatment
To further support your gut health, consider continuing your probiotic regimen for at least one week after completing your course of antibiotics. This can help ensure that your gut microbiome is fully restored.
The Science Behind Probiotics and Antibiotics: What the Research Says
While numerous studies support the use of probiotics during antibiotic treatment, some research also questions the effectiveness of probiotics in restoring gut microbiome diversity. A recent meta-analysis suggested that while probiotics may have some benefits, they did not significantly enhance gut microbiome diversity.
This highlights the need for more research to establish the optimal use of probiotics alongside antibiotics. However, the consensus remains that probiotics can help alleviate some of the common side effects associated with antibiotics, particularly AAD.
Common Side Effects of Probiotics
While probiotics are generally considered safe, some individuals may experience side effects, particularly when starting a new supplement. Possible side effects include:
- Gas and bloating: As your gut adjusts to the new bacteria, you may experience some discomfort initially.
- Digestive upset: Some individuals may notice changes in their bowel habits.
- Rare allergic reactions: Though uncommon, some people may have an allergic reaction to certain probiotic strains.
If you have any underlying health conditions, especially those that compromise your immune system, it’s always best to consult with a healthcare provider before starting probiotics.
Empowering Your Gut Health Journey
At Bala Health, our commitment to gut health extends beyond just providing high-quality probiotics. We believe in empowering our customers through education, transparency, and integrity. Our clinically-backed probiotic is designed to support your gut health and overall wellness effectively.
Are you ready to take the next step in your gut health journey? Start your journey to better gut health with our clinically-backed probiotic!
Furthermore, if you’re looking to understand more about your health and wellness, we invite you to take our 3-minute Weight-Loss Quiz. This personalized quiz will help you kick-start your transformation and tailor a roadmap to better health.
Conclusion
Navigating the world of gut health can feel overwhelming, especially when antibiotics are involved. However, understanding the relationship between antibiotics and probiotics is key to maintaining a healthy gut microbiome. By choosing the right probiotic strains, timing your doses correctly, and continuing your regimen after antibiotic treatment, you can support your gut health effectively.
We hope this article has clarified many of your questions about taking probiotics with antibiotics. Remember, a healthy gut contributes to overall well-being, and with the right approach, you can maintain that balance even during antibiotic treatment.
For a deeper dive into your personalized health journey, take our Weight-Loss Quiz and explore how our probiotics can support your health needs. Shop our clinically-backed probiotic now and feel better from the inside out!
FAQ
1. Can I take probiotics at the same time as antibiotics?
It’s best to take probiotics at least two hours apart from antibiotics to prevent interactions.
2. How long should I continue taking probiotics after finishing antibiotics?
We recommend continuing probiotics for at least one week after completing your antibiotic course to help restore gut health.
3. What are the best probiotic strains to take with antibiotics?
Look for strains like Lactobacillus rhamnosus, Saccharomyces boulardii, and various Bifidobacterium species.
4. Are there any side effects from taking probiotics?
Some individuals may experience mild gas or bloating when starting probiotics, but serious side effects are rare.
5. How can I support my gut health aside from probiotics?
Incorporating a balanced diet rich in prebiotics (like fruits and vegetables) and fermented foods can further support your gut health.
6. Can I take probiotics if I have a compromised immune system?
If you have underlying health conditions or a compromised immune system, it’s best to consult with a healthcare provider before starting probiotics.