Table of Contents
Introduction
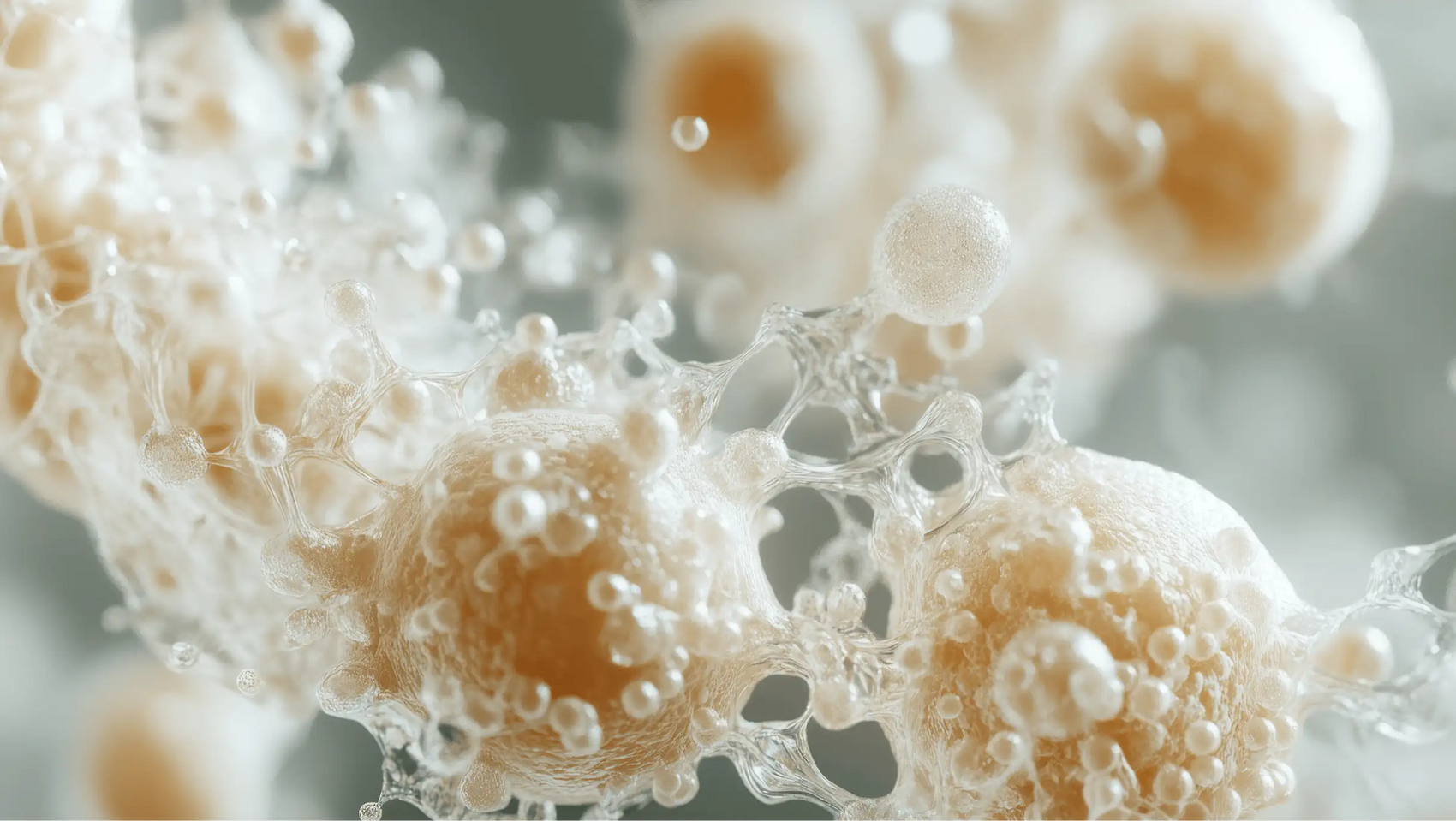
Did you know that the human gut is home to trillions of microorganisms, collectively known as the gut microbiome? This diverse community of bacteria plays a crucial role in our overall health, influencing everything from digestion and metabolism to immune function and even our mood. However, one of the most common medical interventions—antibiotics—can significantly disrupt this delicate balance.
In recent years, we’ve seen a growing awareness of the importance of gut health, largely due to research highlighting the gut-brain axis and its implications for mental and physical wellbeing. As we navigate the complexities of modern healthcare, understanding how antibiotics affect our gut health and what we can do to support recovery is vital.
In this blog post, we will explore the following:
- How antibiotics impact the gut microbiome.
- The long-term consequences of antibiotic use on gut health.
- Strategies to mitigate the negative effects of antibiotics.
- The role of probiotics and prebiotics in gut recovery.
By understanding these aspects, we aim to empower you to make informed decisions about your health and well-being. Are you tired of the confusion and skepticism surrounding gut health? Let’s simplify it together.
At Bala Health, we are committed to transparency and science-backed wellness solutions. Our mission is to help you feel better from the inside out with our clean, functional probiotics. So, let’s dive deeper into the fascinating world of gut health and antibiotics.
The Gut Microbiome: A Brief Overview
Before we delve into the effects of antibiotics, it's essential to understand what the gut microbiome is and why it matters. The gut microbiome refers to the diverse array of microorganisms residing in our intestines, including bacteria, viruses, fungi, and archaea. These microorganisms play several key roles:
- Digestion and Metabolism: They help break down complex carbohydrates and synthesize essential vitamins, such as B vitamins and vitamin K.
- Immune Function: A healthy microbiome supports the immune system by preventing colonization by harmful pathogens.
- Gut Barrier Integrity: Beneficial bacteria help maintain the gut lining, preventing leaky gut syndrome.
- Mental Health: The gut-brain connection means that a balanced microbiome can influence mood and cognitive function.
Given these crucial functions, maintaining a healthy microbiome is essential for overall health. Unfortunately, antibiotics, while life-saving in many cases, can disrupt this delicate ecosystem.
How Antibiotics Affect the Gut Microbiome
Antibiotics are designed to kill or inhibit the growth of bacteria, but they do not discriminate between harmful pathogens and beneficial gut bacteria. This indiscriminate action can lead to several negative consequences:
1. Reduction in Microbial Diversity
One of the most significant impacts of antibiotic use is a decrease in the diversity of the gut microbiome. Research shows that antibiotics can lead to a dramatic reduction in the number of different bacterial species present. This loss of diversity is concerning because a more diverse microbiome is generally associated with better health outcomes.
2. Changes in Bacterial Composition
Antibiotics can alter the composition of the gut microbiome by preferentially killing certain beneficial bacteria. For instance, studies have shown that antibiotics reduce populations of Bacteroidetes and Firmicutes—two groups of bacteria known for their positive effects on health. In their absence, harmful bacteria, such as Clostridioides difficile, may flourish, leading to infections and other health issues.
3. Short- and Long-Term Effects
While some studies indicate that microbial diversity can recover after antibiotic treatment, other research suggests that certain beneficial bacteria may never fully return. A 2017 study found that even a short course of antibiotics could disrupt the gut microbiome for up to a year or more. The effects can be particularly pronounced in vulnerable populations, such as infants and the elderly.
4. Implications for Health
The consequences of antibiotic-induced changes in the gut microbiome can extend beyond gastrointestinal issues. Research links reduced microbial diversity to various health problems, including:
- Gastrointestinal Disorders: Antibiotic use has been associated with conditions like irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD).
- Metabolic Conditions: Studies suggest that antibiotic exposure may increase the risk of obesity and type 2 diabetes.
- Immune Dysfunction: Disruption of gut bacteria can lead to altered immune responses, increasing susceptibility to infections and autoimmune diseases.
Strategies for Recovery After Antibiotic Use
Recognizing the potential negative effects of antibiotics on gut health is the first step toward proactive recovery. Here are several strategies to support the restoration of a healthy gut microbiome:
1. Incorporate Probiotics
Probiotics are live microorganisms that can provide health benefits when consumed in adequate amounts. They help restore the balance of good bacteria in the gut and can be particularly effective in preventing antibiotic-associated diarrhea. At Bala Health, our flagship probiotic is scientifically formulated to support gut health and ease occasional bloating. Feel better from the inside out—subscribe and save on our clinically-backed probiotic now.
2. Include Prebiotics in Your Diet
Prebiotics are non-digestible fibers that feed beneficial gut bacteria. Foods rich in prebiotics include:
- Bananas
- Onions
- Garlic
- Leeks
- Asparagus
- Whole grains
Incorporating these foods into your diet can help stimulate the growth of beneficial bacteria and enhance gut health.
3. Focus on a Whole Foods Diet
A diet rich in diverse, whole foods can support the recovery of the gut microbiome. Emphasize:
- Fruits and vegetables: Aim for a rainbow of colors to ensure a variety of nutrients.
- Fermented foods: Yogurt, kefir, kimchi, sauerkraut, and kombucha can introduce beneficial bacteria into your gut.
- Fiber-rich foods: Foods high in fiber promote the growth of healthy gut bacteria.
4. Stay Hydrated
Drinking plenty of water is essential for overall health, including gut health. Hydration helps maintain the mucosal lining of the intestines and supports the digestive process.
5. Limit Stress
Chronic stress can negatively impact gut health. Incorporating mindfulness practices, such as meditation, yoga, or deep breathing exercises, can help reduce stress levels and support a healthy gut.
6. Avoid Unnecessary Antibiotics
One of the most effective ways to protect your gut health is to avoid unnecessary antibiotic use. Only take antibiotics when prescribed by a healthcare professional and ensure they are the appropriate treatment for your condition.
7. Consider Fecal Microbiota Transplants (FMT)
In severe cases of gut dysbiosis, particularly after recurrent Clostridioides difficile infections, fecal microbiota transplants may be considered. This procedure involves transferring stool from a healthy donor to restore a balanced microbiome.
Conclusion
The impact of antibiotics on gut health is a multifaceted issue that requires careful consideration. While antibiotics are invaluable in treating bacterial infections, their effects on the gut microbiome can have significant and lasting consequences. By understanding these impacts and taking proactive steps to support gut health, we can mitigate the risks associated with antibiotic use.
At Bala Health, we believe in empowering our customers to make informed decisions about their health. Our clean, science-backed probiotics are designed to support your journey to better gut health. If you're ready to take control of your gut health, take our 3-minute Weight-Loss Quiz to find your personalized gut-health roadmap.
Together, we can navigate the complexities of gut health and empower ourselves to feel better from the inside out.
FAQ
Q: Can antibiotics permanently damage my gut microbiome?
A: While some studies show that gut microbiome diversity can recover after antibiotic use, certain beneficial bacteria may not return, leading to potential long-term effects.
Q: How can I support my gut health after taking antibiotics?
A: Incorporate probiotics and prebiotics into your diet, focus on whole foods, stay hydrated, manage stress, and avoid unnecessary antibiotics.
Q: Are all probiotics effective for restoring gut health?
A: Not all probiotics are created equal. It's essential to choose strains that have been clinically studied for their efficacy. Our Bala Health probiotic is designed with this in mind.
Q: How long does it take to restore gut health after antibiotics?
A: Recovery times can vary depending on the individual and the antibiotic used. Some people may experience significant recovery within a few months, while others may take longer.
Q: What should I do if I experience digestive issues after antibiotics?
A: Consult a healthcare professional for guidance. They may recommend dietary changes, probiotics, or further testing to assess your gut health.