Table of Contents
Introduction
Imagine sitting down for a meal, only to feel a wave of discomfort wash over you—not because of what you ate, but due to your stomach's inability to process it properly. This unsettling experience is all too common for those affected by gastroparesis, a condition marked by delayed gastric emptying that can lead to nausea, bloating, and early satiety. This condition affects approximately 4% of the population, with women being disproportionately affected. As we delve into the complexities of managing gastroparesis, understanding the role of gut health becomes crucial.
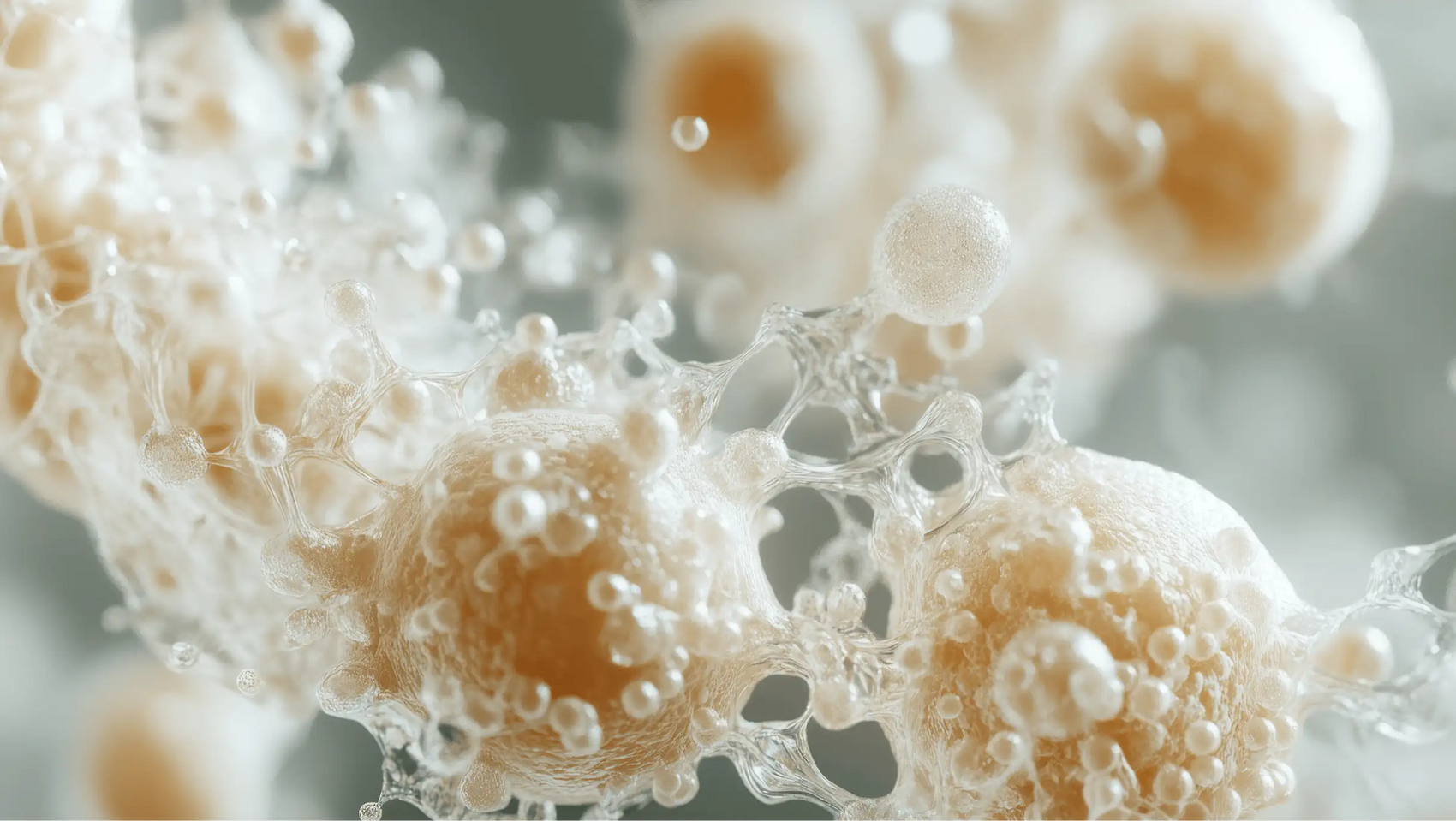
The gut microbiome, a vast community of microorganisms residing in our digestive tract, plays a vital role in our overall well-being. Among these microorganisms, probiotics—often referred to as "good bacteria"—have garnered attention for their potential benefits in various gastrointestinal disorders. This leads us to the pivotal question: Are probiotics good for gastroparesis?
In this post, we will explore the relationship between probiotics and gastroparesis. We’ll discuss how probiotics may influence gastric motility, the underlying mechanisms involved, and the existing research on this topic. By the end of our journey, we aim to provide a comprehensive understanding of whether incorporating probiotics into one’s diet could be beneficial for those suffering from gastroparesis.
What You Will Learn
Together, we will uncover the potential of probiotics in assisting with gastroparesis and how they can form part of a holistic approach to gut health. We will cover the definition of gastroparesis, its symptoms and causes, the importance of gut microbiota, the role of probiotics, and practical recommendations for incorporating them into your routine.
Understanding Gastroparesis: Symptoms and Causes
Gastroparesis is defined as a disorder in which the stomach takes too long to empty its contents. This condition is not due to a blockage but rather involves damage to the vagus nerve, which controls the stomach muscles. When this nerve is impaired, the muscular contractions needed to move food along the digestive tract are disrupted.
Common Symptoms of Gastroparesis
Patients with gastroparesis may experience a variety of symptoms, which can vary in severity:
- Nausea and Vomiting: Many individuals experience a constant feeling of queasiness and may vomit undigested food hours after eating.
- Bloating and Abdominal Pain: The retention of food in the stomach can lead to discomfort and excessive gas.
- Early Satiety: People with gastroparesis often feel full after eating only a small amount of food.
- Weight Loss and Malnutrition: Due to difficulties in eating and absorbing nutrients, individuals may experience unintentional weight loss.
Causes of Gastroparesis
The causes of gastroparesis can be multifaceted and include:
- Diabetes: About 30% of people with diabetes experience gastroparesis, making it a significant concern in diabetic care.
- Post-Surgical Complications: Surgery involving the stomach or vagus nerve can lead to gastroparesis.
- Certain Medications: Some medications, particularly those that affect stomach motility, can contribute to the condition.
- Viral Infections: Certain viral infections may trigger or exacerbate symptoms.
The Gut Microbiome and Its Importance
The gut microbiome consists of trillions of microorganisms, including bacteria, viruses, fungi, and other microbes. This diverse ecosystem plays a critical role in our health, influencing digestion, metabolism, immune function, and even mental well-being.
The Role of Gut Microbiota
An imbalance in gut microbiota, known as dysbiosis, can lead to various gastrointestinal disorders, including irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD). Recent studies suggest that dysbiosis may also be implicated in gastroparesis. Alterations in the gut microbiota can affect the gut-brain axis, a complex communication network linking the gut and the brain, influencing gut motility and overall digestive health.
Probiotics: What Are They?
Probiotics are live microorganisms that, when consumed in adequate amounts, confer health benefits to the host. They can be found in fermented foods such as yogurt, kefir, sauerkraut, and in dietary supplements. Different strains of probiotics, including Lactobacillus and Bifidobacterium, have been associated with various health benefits, particularly in supporting digestive health and restoring the balance of gut microbiota.
How Probiotics Work
Understanding how probiotics work is crucial in evaluating their potential benefits for gastroparesis. Probiotics may enhance gut motility, improve the gut's immune response, and reduce inflammation—all factors that could be beneficial for individuals suffering from delayed gastric emptying.
The Connection Between Probiotics and Gastroparesis
Given the potential benefits of probiotics on gut health, researchers have begun to explore their impact on gastroparesis. Some studies indicate that specific probiotic strains may help improve gastric emptying times, suggesting a positive correlation between probiotic intake and alleviation of some gastroparesis symptoms.
Current Research Findings
- Improvement in Gastric Emptying: A study found that participants taking a multi-strain Lactobacillus probiotic experienced improved gastric emptying times compared to those who did not take the probiotic. This suggests that certain probiotics may enhance digestive motility.
- Symptom Relief: Clinical trials have shown that probiotics may help alleviate symptoms such as bloating and abdominal discomfort, common in gastroparesis. By promoting a healthier gut microbiome, probiotics may reduce the severity of symptoms associated with this condition.
- Influence on Gut-Brain Axis: Probiotics are believed to interact with the gut-brain axis, potentially influencing the signals that regulate gastric motility. This interplay could be particularly beneficial for individuals with gastroparesis, as it might help restore some of the disrupted communication between the gut and the nervous system.
Case Studies and Anecdotal Evidence
While large-scale clinical trials are still needed, anecdotal evidence from individuals with gastroparesis suggests that probiotics may offer symptom relief. Many patients report improvements in their overall digestive health and a reduction in discomfort when incorporating probiotics into their diets.
Practical Recommendations for Incorporating Probiotics
If you’re considering adding probiotics to your management plan for gastroparesis, here are some practical steps to keep in mind:
- Choose the Right Strain: Not all probiotics are created equal. Certain strains, such as Lactobacillus rhamnosus and Bifidobacterium bifidum, have shown promise in improving gut health. Look for targeted formulations that address specific digestive concerns.
- Monitor Your Symptoms: Keep track of any changes in your symptoms after introducing probiotics into your routine. If you notice improvements, discuss them with your healthcare provider to determine the best course of action.
- Incorporate Probiotic Foods: In addition to supplements, consider adding probiotic-rich foods to your diet. Fermented foods like yogurt, kefir, and sauerkraut can be delicious and beneficial additions to your meals.
Conclusion
The relationship between probiotics and gastroparesis is an area of growing interest and research. While current evidence suggests that probiotics may help improve gastric motility and alleviate some symptoms of gastroparesis, more extensive clinical studies are needed to confirm these benefits. At Bala Health, we believe that wellness starts with trust, and we are committed to providing high-quality, science-backed probiotics that empower our community to take control of their health.
If you’re interested in exploring how probiotics might fit into your wellness journey, consider taking our Weight-Loss Quiz to discover personalized recommendations tailored to your needs. Additionally, explore our Bala Health Probiotic to support your gut health journey. Together, let’s embark on a journey toward better gut health!
FAQ
- Can probiotics completely cure gastroparesis? Probiotics are not a cure for gastroparesis, but they may help improve symptoms and support gut health. It’s essential to view them as a complementary approach within a broader management plan.
- How long does it take to see results from probiotics? Results can vary depending on the individual and the specific probiotic strain used. Some people may notice improvements within a few days, while others may require weeks of consistent use.
- Are there any side effects associated with probiotics? Most people tolerate probiotics well, but some may experience mild side effects such as bloating, gas, or digestive discomfort. It’s advisable to start with a lower dose and increase gradually.
- Should I stop taking my regular medications if I start probiotics? Always consult your healthcare provider before making any changes to your medication regimen. Probiotics should complement your existing treatment plan rather than replace any prescribed medications.
- Where can I find high-quality probiotics? Look for reputable brands that offer transparency about their ingredients and manufacturing processes. At Bala Health, we prioritize quality and provide supplements with no hidden ingredients.
By understanding the role of probiotics in managing symptoms associated with gastroparesis, we can all take steps toward better digestive health. Let’s work together to empower ourselves and our community in the journey toward wellness!